Finding the Right Prioritization Model

By JUSTIN SPECTOR
Restrictions on elective surgical volume in hospitals across the United States are causing a dilemma heretofore unseen in the American healthcare system. Surgeons across services have large and growing backlogs of elective surgeries in an environment where operating room (OR) capacity is restricted due to availability of inpatient beds, personal protective equipment (PPE), staffing, and many other constraints. Fortunately, the U.S. is not the first country to experience and deal with this situation; for many countries, this is the normal state of medicine.
By combining the accumulated experience of health systems around the world with cutting-edge technologies, it is possible to make this crisis manageable for perioperative leadership and, potentially, to improve upon the preexisting models for managing OR time.
The first step in creating an equitable system that can garner widespread buy-in is to agree upon a method for categorizing cases into priority levels. Choosing a system with strong academic backing will help to reduce the influence of intra-hospital politics from derailing the process before it can begin.
Why Cases Should Be Prioritized
If your hospital has a mix of surgeons who perform highly time-sensitive cases — cases where patient quality of life is substantially impacted — as well as cases with minor health or quality of life outcomes, it is important to make sure there will be enough capacity to get the higher urgency cases done within a reasonable amount of time. This allows cases in the backlog to be balanced against new cases that are yet to be scheduled and will help to optimize the flow of patients through the OR.
Case Prioritization Best Practices
The most important feature of a prioritization model is for it to be something your hospital, surgeons and schedulers will be able to understand and be willing to use. For this reason, we have excluded systems that are difficult to implement, such as that used by the Department of Veterans Affairs. The models included, with one exception, have long track records of success, and any hospital should be able to implement them.
Another important consideration in prioritization is what factors you want to consider. These can be broken into three major categories: clinical urgency, risk to the patient, and risk to the hospital. Risk to the patient would include factors such as ASA score, age and any complicating conditions that would make the patient especially at risk if infected with SARS-CoV-2. Clinical urgency — the rate at which the patient’s condition is worsening and the patient’s ability to wait for surgery — is the most straightforward. Finally, risk to the hospital takes into account many factors such as the risk of the patient spreading infection to hospital staff and other patients, their likelihood of needing an ICU bed and blood, and the amount of PPE needed for the case. Each hospital will need to place a different amount of emphasis on each category.
Four Prominent Case Prioritization Models
Descriptive – Surgical Waiting List Info System (SWALIS): SWALIS is a system based on the Italian government’s case prioritization guidelines that solely take into account clinical urgency to assign a case one of five levels, and each priority level is associated with a maximum time before treatment (MTBT). This model is easy to understand and requires minimal administrative oversight, but it does not take into account other factors such as equipment needs and risk to the patient and hospital. Because of the ease of implementation and clarity of the segmentation, this is a favored model.
Prescriptive – British Columbia Ministry of Health Surgical Patient Registry (SPR): The model used in British Columbia, Canada, is similar to the Italian model in that it divides cases into groups by clinical urgency. However, instead of the surgeon subjectively determining the priority level, this model prescribes a level based on the procedure. This system is especially effective if it will be difficult to instruct your clinics on the prioritization methodology but requires a lot of decisions to be made centrally to determine the priority for each procedure and any modifiers that need to be considered.
- Patient Prioritization Codes: Overview
- Surgical Wait Time Strategy
- Surgical Wait Times – Procedures A-Z
- Dental Surgery ‐ Adult – BC List of Patient Condition and Diagnosis Descriptions
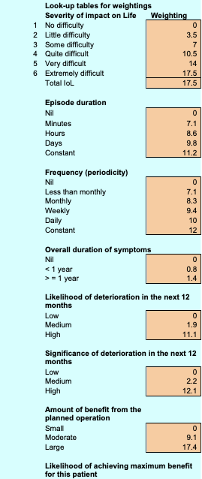
Qualitative Patient Need – General Surgery Prioritization Tool (GSPT): New Zealand was one of the first countries to implement clinical priority assessment criteria (CPAC) nationwide. One CPAC tool being used is the GSPT. It uses a 0-100 scale for each case based on aspects of the impact on the patient’s quality of life and health to determine a relative priority. (See Appendix)
Qualitative Multifactor – Medically Necessary, Time-Sensitive (MeNTS): Published in the Journal of the American College of Surgeons, this system uses a mix of subjective and objective scores in different categories to create a cumulative score between 21 and 105. Higher scores equate to a greater risk to reward for the procedure. The process of scoring each case requires 21 factors to be rated on a scale of 1 to 5, making this best suited to systems with strong admin staff who can complete these evaluations for each case.
Choosing the Right Model
The two most important factors when designing a prioritization model for your hospital or system are consistency and compliance. It is important that across surgeons and service lines there is an understanding of what priority level is appropriate and that those are in line with leadership’s intent. It is also important to consider the ease of use as models that require too much work per individual case may be ignored or half-heartedly complied with.
As there has been little national or state-level guidance on this subject, each hospital organization has a great deal of leeway to choose a method that fits their unique needs.
Other Considerations
If your hospital is constrained on beds, PPE, blood or any other surgical input, consider adding these as factors in your prioritization system. For example, if PPE is a constraint, it’s important to balance case lengths as shorter cases result in more PPE use throughout a surgery day. Similarly, if inpatient beds are limited, you may want to set a threshold on the total number of cases that require greater than six hours of in-bed recovery time. This is an area where web-based tools excel due to their ability to leverage sophisticated packing algorithms.
Translating Priority Scores Into Surgery Dates
In the American healthcare system, surgical schedules are built around block allocation. This means that each case’s score is not enough to determine when it should be performed since the surgeons will not be coming in to do just one case. Each surgeon or department’s entire backlog should be considered to determine how surgical time should be distributed.
The challenge is to balance priority against wait time and overall backlog volume. While certain service lines may only have low- to medium-priority cases, if their caseload is sufficient, then they should be given time even within the first few weeks of opening up elective booking. Using a scoring system for each case that takes into account wait time, along with determining the MTBT for each priority category, it is possible to formulate how much time each surgeon or service should receive each week. Because surgeons’ waitlists are constantly changing, it is useful to repeat this exercise at a weekly or biweekly cadence to ensure optimal distribution.
Further Reading
Below are academic papers that discuss the importance and process of prioritization that may also be useful. The author would like to thank Dr. James Caldwell, director of surgical services, Parkview Medical Center, for his assistance in compiling this information.
Edwards RT. Points for pain: waiting list priority scoring systems. BMJ. 1999;318(7181):412–414; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1114887/
Curtis AJ, Russell COH, Stoelwinder JU, McNeil JJ (2010). Waiting Lists and Elective Surgery: Ordering the Queue. Medical Journal of Australia. 192: 217-220. doi:10.5694/j.1326-5377.2010.tb03482.x; https://www.ncbi.nlm.nih.gov/pubmed/20170460
COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures (Online March 17, 2020); https://www.facs.org/covid-19/clinical-guidance/triage
Mullen P M (2003). Prioritising waiting lists: how and why? European Journal of Operational Research, 150(1), 32–45. doi: 10.1016/S0377-2217(02)00779-8; https://www.sciencedirect.com/science/article/abs/pii/S0377221702007798?via%3Dihub
Davis B, Johnson SR. Real-time priority scoring system must be used for prioritisation on waiting lists. BMJ. 1999;318(7199):1699. doi:10.1136/bmj.318.7199.1699; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1116039/
Testi A, Tanfani E, Valente R, Ansaldo GL, Torre GC. Prioritizing Surgical Waiting Lists. Journal of Evaluation in Clinical Practice. 2006; ISSN 1356-1294; https://pubmed.ncbi.nlm.nih.gov/18211645/
Appendix
Scoring system for NZ, GSPT
Justin Spector is a product manager at LeanTaaS where he is continuously enhancing ways to help hospitals ease access to OR time and optimize OR utilization.
from The Health Care Blog https://ift.tt/3fx46el
via IFTTT

No comments:
Post a Comment