Prior authorization is a requirement that health plans require physicians to obtain plan approval in order to prescribe a patient a given medication. Prior authorizations may be put in place to insure medications are not used inappropriately or for payers to try to reduce cost. While prior authorization may help save money, delays in the prior authorization approvals frustrate patients and clinicians. ICER reports:
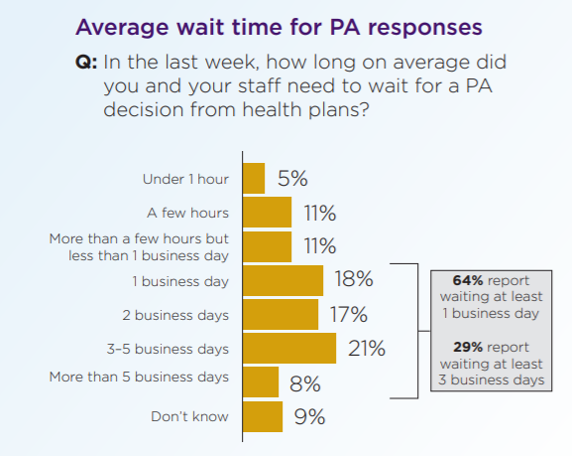
… a 2018 Physician Survey conducted by the AMA on prior authorization found that 65% of providers had to wait, on average, at least one business day within the past week before receiving a prior authorization decision from a health plan and 26% of providers waited three business days or more. It should also always be remembered that prior authorization protocols impose an administrative burden on patients and clinicians that can, by itself, pose a risk to fair access. Clinicians have cited the burden of prior authorization as one of the leading causes of burnout.
An AMA survey states that 24% of physicians report that a PA has lead to a serious patient adverse event. Below are some statistics from the 2019 AMA PA Physician Survey.

Sources:
- American Medical Association. 2019 AMA Prior Authorization (PA) Physician Survey. June 2020.https://www.ama-assn.org/system/files/2020-06/prior-authorization-survey-2019.pdf
- Berg S. The 12 factors that drive up physician burnout. Physician Health. 2020. https://www.ama-assn.org/practice-management/physician-health/12-factors-drive-physicianburnout
from Healthcare Economist https://ift.tt/33D04hc
via IFTTT

No comments:
Post a Comment