


By VINCE KURAITIS, ERIC PERAKSLIS, and DEVEN McGRAW
This piece is part of the series “The Health Data Goldilocks Dilemma: Sharing? Privacy? Both?” which explores whether it’s possible to advance interoperability while maintaining privacy. Check out other pieces in the series here.
A worldwide dialog about COVID-19 contact tracing is underway. Even under the best of circumstances, the contact tracing process can be difficult, time-consuming, labor-intensive, and invasive — requiring rigorous, methodical execution and follow-up.
COVID-19 throws curve balls at the already difficult process of contact tracing. In this post we will provide some basic background on contact tracing and will list and describe 10 challenges that make contact tracing of COVID-19 exceptionally difficult. The 10 unique challenges are:
1) COVID-19 is Highly Contagious and Deadly
2) Contact Tracing is Becoming Politicized
3) We Lack Scientific Understanding of COVID-19
4) Presymptomatic Patients Can Spread COVID-19
5) Asymptomatic Patients Can Spread COVID-19
6) Contact Tracing is Dependent on Availability of Testing
7) Contact Tracing is Dependent on New, Extensive Funding
8) Contact Tracing is Dependent on an “Army of Tracers” and Massive Support for Patients
9 ) The Role of Technology is Unclear — Is it Critical Support or a Distraction?
10) The U.S. Response Has Been Fragmented and Inconsistent
The thrust of this post is about traditional boots-on-the-ground contact tracing conducted by public health agencies. We will touch on a few aspects of digital contact tracing (e.g., smartphone apps), but we’ll go into much more depth on digital contact tracing in future posts.
How does contact tracing relate to the theme of this series — The Health Data Goldilocks Dilemma? It’s about obtaining the right amount and types of information — not too much, not too little. Not too much data so that privacy rights or civil liberties are infringed, or that contact tracers are overwhelmed with useless data; not too little data so that public health agencies aren’t handcuffed in protecting our safety in tracing COVID-19 cases.
Contact Tracing 101
Contact tracing is “an old-school epidemiological tool for studying and documenting the chains of transmission of infectious diseases during outbreaks.”

The Box It In framework (shown above) is one way of describing necessary follow-on activities in controlling COVID-19: “After flattening the curve, the next step is to box the virus in by implementing four essential actions… 1) Expand and prioritize testing, 2) Isolate infected people to prevent disease spread, 3) Identify contacts who infected people might have exposed, and 4) Quarantine contacts.”
Dr. Tom Frieden, former director of U.S. Centers for Disease Control and Prevention (CDC), described how contact tracing fits within the overall Box It In strategy:
3. Trace contacts of people with COVID-19 through hundreds of thousands of contact tracers. To get ahead of the pandemic, we must trace all the contacts of infected people and warn them of their exposure to the coronavirus so they don’t spread the infection. For this unprecedented effort, we need to build, train, and supervise a corps of contact tracers nationwide and address the public’s concerns about confidentiality and privacy. Some technologies may be able to improve efficiency—although new digital tools are likely to supplement but not supplant traditional public health processes.
There are many excellent resources which provide additional background on the COVID-19 contact tracing process, see e.g., Johns Hopkins, the CDC, Duke Forge, or Pro-Publica.
10 Unique Contact Tracing Challenges of COVID19
Let’s examine some of the reasons why contact tracing is especially challenging for the coronavirus pandemic.
1) COVID-19 is Highly Contagious and Deadly
As of June 10, more than 7.2 million cases of COVID-19 have been reported worldwide, as well as more than 412,000 deaths.
Contact tracing is complicated due to the potential to spread the disease beyond “known” contacts, e.g., through sneezing in public, casual contacts, or spreading the virus on surfaces. Different pathogens have different “reproductive numbers” (called R0 or R-naught), which is the average number of infections one person transmits. The R0 for the SARS-CoV-2 virus is thought to be between 2–3. Research to-date indicates that COVID-19 spreads more easily and has a higher death rate than the flu.
2) Contact Tracing is Becoming Politicized
We see at least four overlapping aspects of how COVID-19 contact tracing is becoming politicized: 1) perceptions of interference with civil liberties, 2) perceptions of loss of privacy rights, 3) recent social unrest amplifying distrust of government, and 4) controversy over the hiring of private firms.
Contact tracing originates from a time when the world was less populated and people traveled less frequently. In the past, contact tracing initiatives more typically dealt with smaller numbers of diseased people who were geographically confined, for example people with measles, sexually transmitted diseases, or tuberculosis. Contact tracing typically occurred without the general public even being aware of it.
COVID-19 is different. It has spread internationally and is present in all 50 U.S. states. The need for extensive contact tracing is being characterized as akin to governmental mass surveillance.
An article in Politico examined the contact tracing program in New York City and how recent social unrest has increased preexisting distrust of government. “After a week of chaotic protests against the police following the killing of George Floyd, suspicion between residents and government authorities has only grown, community leaders say.” The takeaway: “Privacy fears threaten New York City’s coronavirus tracing efforts”.
Lastly…hiring private firms to assist in contact tracing brings another layer of controversy.
3) We Lack Scientific Understanding of COVID-19
The headline in the Washington Post proclaimed: “The science on coronavirus is still murky”.
“Modelers gave varying predictions for how many infections and deaths could result. Epidemiologists are still debating the true infection and fatality rates. Medical professionals don’t fully understand why the virus hits some hard and not others, and the extent to which children without symptoms can pass it along.”
One result has been confusing and sometimes contradictory guidance from governments.
4) Presymptomatic Patients Can Spread COVID-19
The CDC estimates that 40% of coronavirus transmission is occurring before people feel sick. Patients that are presymptomatic or asymptomatic can still spread the virus to others, yet are unlikely to seek medical attention. This makes it exceedingly difficult to trace chains of transmission.
The New York Times reported that “Someone working in a restaurant or factory may have dozens or even hundreds of contacts. In China’s Sichuan Province, for example, each known case had an average of 45 contacts.”
The large number of potential contacts further complicates the contact tracing process. A Johns Hopkins Center for Health Security report noted that “COVID-19 can cause large outbreaks quickly, so even 1 missed case can significantly undermine control efforts.”
5) Asymptomatic Patients Can Spread COVID-19
CDC’s best estimate is that 35% of coronavirus patients don’t have symptoms. Dr. Andy Slavitt, former head of the Centers for Medicare and Medicaid Services, discussed implications:
“The picture of a large number of asymptomatic hosts is a chilling one. One asymptomatic spreader can spread Covid-19 to 9,537 patients in 40 days. (Using 10 generations & r0 of 2.5). If 40% of those people have no symptoms, the impetus for them to continue to stay home is lower.”
There is potential for a large number of presymptomatic or asymptomatic cases to simply overwhelm contact tracing programs. A mathematical model developed by Ferreti, et. al. and published in Science estimated that “presymptomatic transmissions alone are almost sufficient to sustain epidemic growth”.
6) Contact Tracing is Dependent on Availability of Testing
The success of contact tracing programs is dependent on numerous external factors, many of which are beyond the control of contact tracers.
Once a close contact is identified, they should be tested for the virus. Test and material shortages were widespread in the early stages of the COVID19 pandemic and persist today. Future shortages would negatively impact the effectiveness of contact tracing programs.
7) Contact Tracing is Dependent on New, Extensive Funding
While there have been numerous proposals to fund federal initiatives for contact tracing, to-date the states are acting independently to develop their own contact tracing programs.
How much funding is needed? Proposals have been all over the map. Some examples:
- A Johns Hopkins Center for Health Security report proposed that “Congress will need to appropriate approximately $3.6 billion in emergency funding to state and territorial health departments.”
- A bipartisan proposal from public health leaders requested $46.5 billion. This included $12 billion to expand the contact tracing workforce.
- A House of Representatives bill proposed $75 billion to expand testing and contact tracing.
We are not aware of a comprehensive analysis of how much states are planning to spend on their contact tracing programs.
8) Contact Tracing is Dependent on an “Army of Tracers” and Massive Support for Patients
How many contact tracers will be needed in the U.S.? Estimates range from 100,000 to 300,000.
Where are we today? An NPR survey conducted in late April found that “states reported having at least 11,142 contact tracers working now.”
#TestAndTrace is a private organization covering contact tracing progress in the U.S. They report that as of June 5 the U.S. states collectively are planning to hire 64,717 tracers.
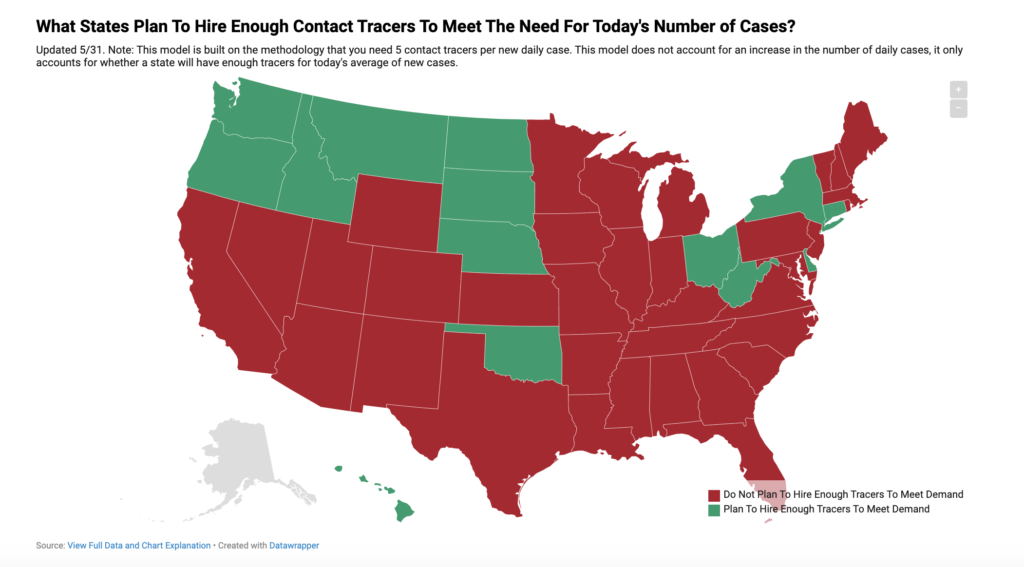
Based on the #TestAndTrace model, today only 12 states are planning to hire enough contact tracers to meet projected needs (see the graphic below).
Hiring tracers is only a first step. The previously referenced bipartisan proposal included funding recommendations of $4.5 billion for “voluntary self-isolation facilities utilizing vacant hotels” and $30 billion for “income support for voluntary self-isolation”.
“If you can’t provide any support, whether that is food delivery, child care, or a referral to a facility, the likelihood you will prevent transmission within the home, and perhaps in the workplace, is close to zero.” — KJ Seung, M.D., Infectious Disease Specialist and Chief of Strategy and Policy, Massachusetts COVID Response group
9) The Role of Technology is Unclear — Is it Critical Support or a Distraction?
You’ve probably read that Apple and Google have a joint initiative for an “exposure notification” app platform to assist individuals and public health agencies in broader contact tracing initiatives. Across the world, there are 80+ apps under development — many of which will be compatible with the Apple/Google platform.
However…many public health leaders are skeptical. Dr. Tom Frieden articulated the apprehensions: “There is potential for these tools but they are unproven, and they are something of a distraction.”
For now, we simply wanted to flag the issue around the value of technology. We’ll have more to say in future posts.
10) The U.S. Response Has Been Fragmented and Inconsistent
The federal government has avoided a centralized role in combatting COVID-19. Most of the efforts have been decentralized and led by individual states.
One example of the fragmentation: an article by Sara Morrison in Recode describes disparate digital contact tracing efforts in various states, including Alabama, North Dakota, South Carolina, Maryland, Arkansas, Idaho, Pennsylvania, Hawaii, Washington and New York.
Conclusion
The story of COVID-19 contact tracing is still in progress, and it’s not clear whether the ending will be success or failure. We hope that this essay has added depth to the opening words “Contact tracing for COVID-19 will be the most complex health investigation ever”.
Vince Kuraitis, JD/MBA (@VinceKuraitis) is an independent healthcare strategy consultant with over 30 years’ experience across 150+ healthcare organizations. He blogs at e-CareManagement.com.
Eric D. Perakslis, PhD (@eperakslis) is a Rubenstein Fellow at Duke University.
Deven McGraw , JD, MPH, LLM (@healthprivacy) is the Chief Regulatory Officer at Ciitizen (and former official at OCR and ONC). She blogs at ciitizen.com.
from The Health Care Blog https://ift.tt/3hpVPdF
via IFTTT

No comments:
Post a Comment